Advances in repair of the shoulder’s ball-and-socket joint are making partial joint replacement rather than total joint replacement a more viable option for a growing number of patients. Moreover, this type of joint replacement is ideal for the growing movement toward outpatient surgery.
Partial shoulder joint replacement, particularly with a stemless implant is less invasive than total joint replacement, preserves natural bone, allows for quicker recovery and, thanks to new technologies, is becoming an increasingly successful, long-term solution for disorders that cause shoulder pain and loss of function.
One of those “new technologies” is the Catalyst CSR Total Shoulder System, featuring a stemless, nonspherical implant and patented instrumentation that can be used for partial or total joint replacements for patients of all ages. The implant’s accuracy has been found to recreate a shoulder’s natural center of rotation better, which could minimize risk of failed joint repairs caused by misaligned shoulder implants.
Until now, total joint replacement has been the gold standard for treating shoulder-joint problems that have not responded to conservative therapies. But during the past several years, we have seen the emergence of revolutionary technologies like the Catalyst CSR system. These advanced tools allow us as surgeons to restore the biomechanics of the shoulder with minimally invasive, bone-sparing approaches on an outpatient basis.
Indeed, mounting research evidence suggests that partial shoulder replacement, where only the “ball” part of the ball-and-socket joint is replaced, may be a preferred alternative for maintaining shoulder-joint viability in more active and athletic patients. As these patients maintain their activity and their joint implants wear, they may require future joint surgery, which will be much more easily and successfully performed because their earlier procedure with an implant like the Catalyst CSR has left more of their natural bone intact.
Injury, osteoarthritis, post-trauma arthritis and avascular necrosis (reduced blood flow to the shoulder causing deterioration of bone) are all disorders that can compromise shoulder-joint cartilage. It is this cartilage that creates the smooth surface on which the ball at the top of the forearm — the humerus — can glide readily within the shoulder blade socket, or glenoid. Loss of this cartilage leads to shoulder pain, swelling, stiffness and decreased range of motion.
Total joint replacement requires cutting away bone to accommodate an implant with a stem that anchors it at the top of the humerus and replacing scapula bone with a prosthesis. In a partial joint replacement procedure with a stemless implant, the surgeon simply clears the diseased area from the ball of the humerus and then caps it with a metallic (cobalt chromium) component that fits into the glenoid socket, restoring the normal anatomy of the joint. In some instances, the surgeon may have to reshape a damaged glenoid.
In a 2019 issue of the Journal of Shoulder and Elbow Arthroplasty, scientists report positive results in new shoulder replacement techniques that rely on specially designed, nonspherical elements — like that provided by the Catalyst system. These implants, authors say, cap the ball at the top of a diseased forearm bone — the humerus — with high precision, preserving the bone’s anatomical relationship with the glenoid, the socket of the shoulder blade and allowing little deviation of the joint during shoulder movement.
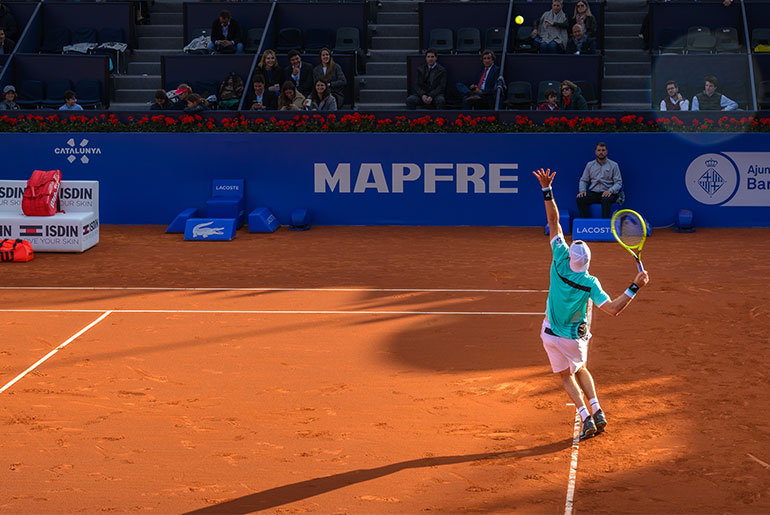
Other advantages of partial shoulder replacement: The procedure is more conservative than total joint replacement, requires a smaller incision, results in less pain, offers quicker recovery and the implant may prolong the function of the joint and help the patient avoid future total shoulder joint replacement. Patients who undergo partial shoulder replacement with a stemless implant are driving a car within a matter of weeks and, within a few months, back to golfing, tennis or other athletic activities.
Not every shoulder patient is a candidate for partial joint replacement, however. Total joint replacement or reverse shoulder arthroplasty may be necessary if the patient is of advanced age or the shoulder disorder involves a rotator cuff tear; structural damage — like a fracture — to the ball-and-socket joint; or presence of extensive disease, including inflammatory arthritis, osteonecrosis and post-injury degeneration of the joint.
Alejandro Badia, M.D., FACS, is a hand and upper-limb surgeon and founder of Badia Hand to Shoulder Center and OrthoNOW, a network of walk-in orthopedic centers. He is the author of “Healthcare From the Trenches.” For more, visit orthonowcare.com and for more on Catalyst OrthoScience, visit CatalystOrtho.com.